Last time we discussed the effects of blood pressure determinants on blood pressure, in essence stating how these determinants control blood pressure. In this last installment on blood pressure, we’ll seek to get a clearer understanding of the measures the body takes physiologically to control blood pressure.
Defining Short- and Long- Term Control Measures
Mean arterial pressure is constantly monitored by baroreceptors (pressure sensors) within the circulatory system. Multiple reflex responses are initiated to return mean arterial pressure to its normal value when deviations from the norm are detected.
Short-term (within seconds) adjustments are made by alterations in Cardiac Output (CO) and total peripheral resistance, mediated by means of autonomic nervous system influences on the heart, veins, and arterioles.
Long-term (requiring minutes to days) control involves adjusting total blood volume by restoring normal salt and water balance through mechanisms that regulate urine output and thirst. The size of total blood volume, in turn, has a profound effect on cardiac output and mean arterial pressure.
Let us now focus on the short-term mechanism involved in the ongoing regulation of this pressure, specifically the Baroreceptor Reflex mechanism.
The Baroreceptor Reflex Mechanism
What Triggers the Baroreceptor Reflex?
Any change in mean arterial pressure triggers an autonomically mediated baroreceptor reflex that influences the heart and blood vessels to adjust CO and Total Peripheral Resistance (TPR) in an attempt to restore blood pressure to normal.
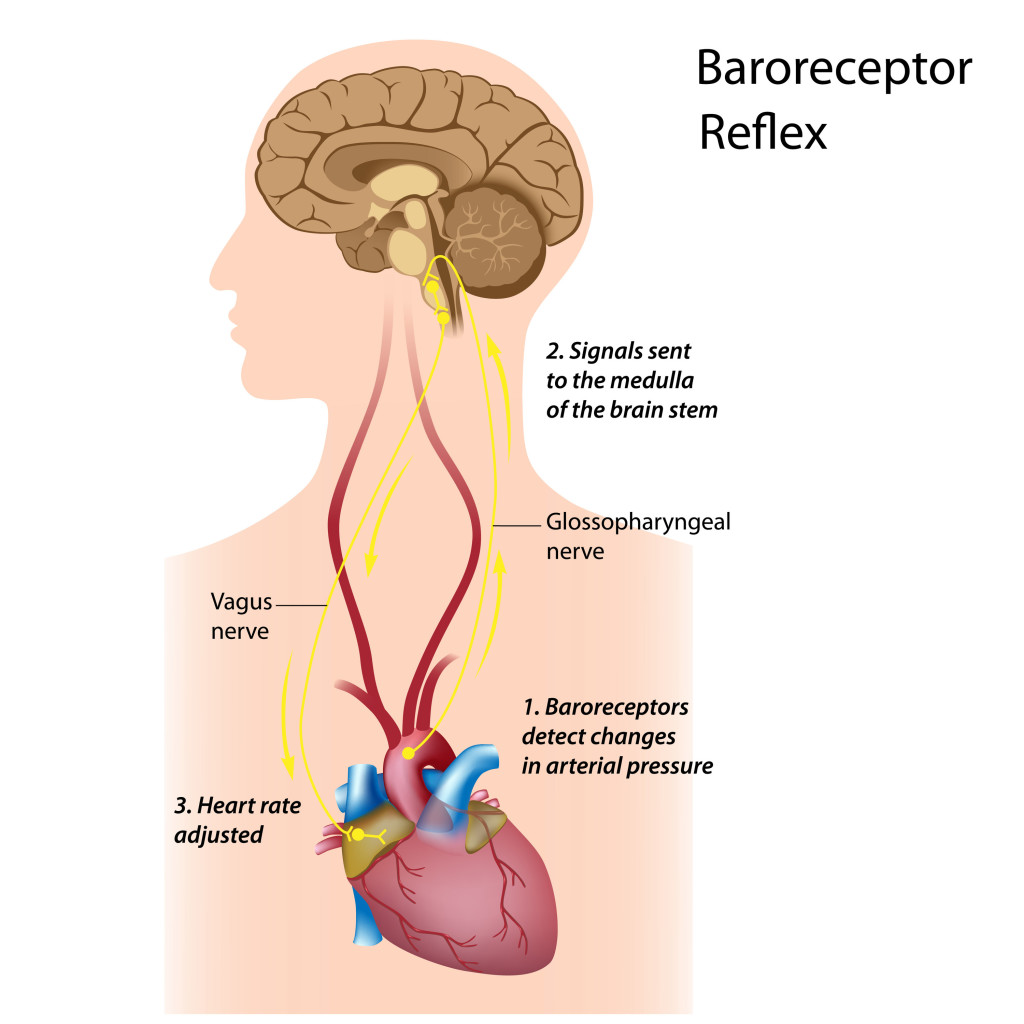
As with any reflex in the body, the baroreceptor reflex includes a receptor, an afferent pathway, an integrating center, an efferent pathway, and effector organs.
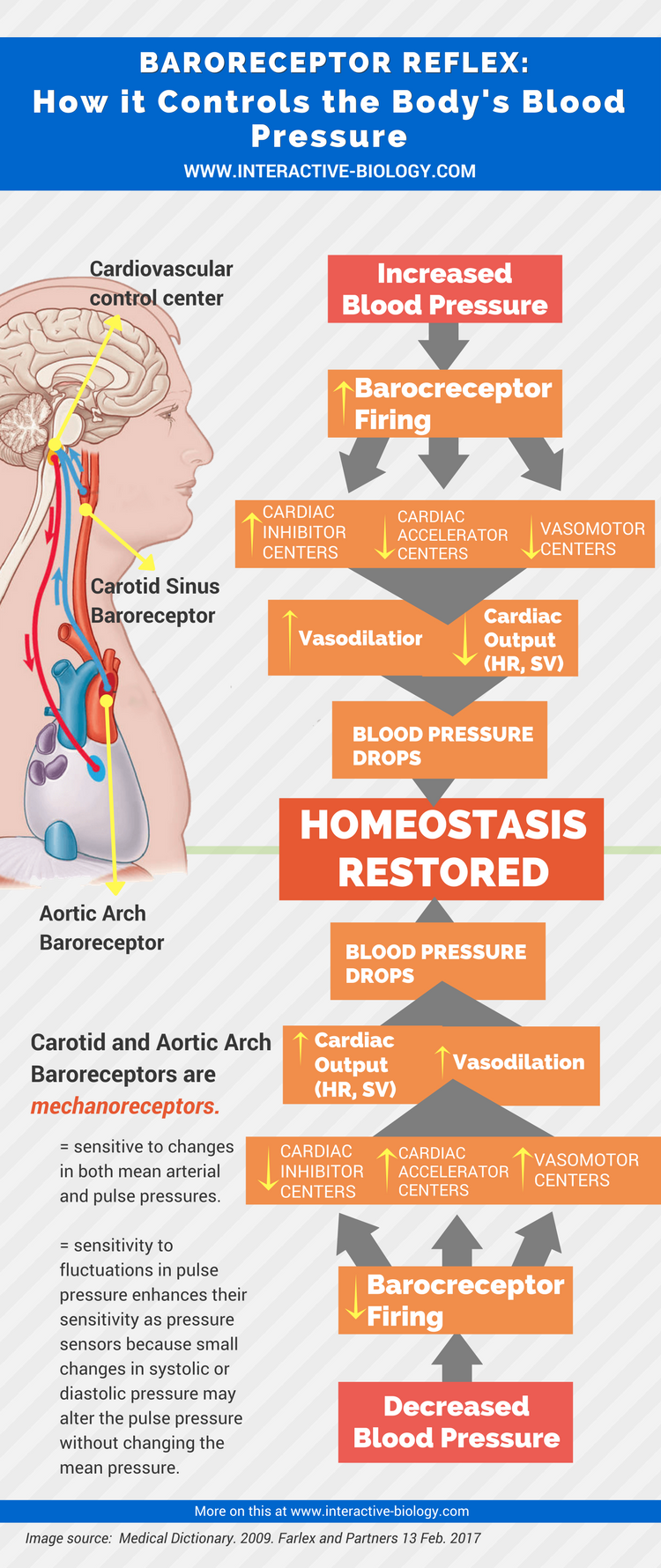
The two most important receptors involved, that we said in the last article, in the moment-to-moment regulation of blood pressure are the carotid sinus and aortic arch baroreceptors.
These are mechanoreceptors, which are sensitive to changes in both mean arterial and pulse pressure. Their sensitivity to fluctuations in pulse pressure enhances their sensitivity as pressure sensors because small changes in systolic or diastolic pressure may alter the pulse pressure without changing the mean pressure.
Baroreceptor Locations in the Body
The locations of these baroreceptors are strategic in order to provide critical information about arterial and blood pressure in the vessels leading to the brain – the carotid sinus- and in the major arterial trunk before it diverges into its branches to supply the rest of the body – the aortic arch.
The baroreceptors constantly provide information about mean arterial pressure; in other words, they continuously generate action potentials in response to the ongoing pressure within the arteries. When arterial pressure – whether it be mean or pulse pressure – increases, the receptor potential of these baroreceptors increases thus increasing the rate of firing in the corresponding afferent neurons. Conversely, a decrease in the mean arterial pressure slows the rate of firing generated by the afferent neurons by the baroreceptors.
The integrating center that receives the afferent impulses about the state of mean arterial pressures is the Cardiovascular control center, which is located in the medulla within the brain stem.
The efferent pathway is the autonomic nervous system. The cardiovascular control center alters the ration between sympathetic and parasympathetic activity to the effector organs (heart and blood vessels).
To put all the pieces of the baroreceptor reflex together we will trace the reflex activity that compensates for an elevation or fall in blood pressure.
How the Baroreceptor Reflex Works
If for any reason at all the mean arterial pressures rises above normal, the carotid sinus and aortic arch baroreceptors increase the rate of firing in their respective afferent neurons. On being informed by an increased afferent firing that the blood pressure has become too high, the cardiovascular control center responds by decreasing sympathetic and increasing parasympathetic activity to the cardiovascular system.
These efferent signals decrease heart rate, decrease stroke volume and produce arteriolar and venous vasodilation, which in turn leads to a decrease in CO and a decrease in TPR, with an ensuing fall in blood pressure back toward normal.
Contrariwise, when blood pressure falls below normal, baroreceptor activity decreases, inducing the cardiovascular center to increase sympathetic cardiac and vasoconstrictor nerve activity while decreasing its parasympathetic output.
This efferent pattern of activity leads to an increase in heart rate and stroke volume, coupled with arteriolar and venous vasoconstriction. These changes increase both CO and TPR, raising blood pressure to normal levels.
Infographic
i feel like some info is lacking…..how are these pressures generated?
can you please explain the conducting system of the heart
How does the body control the blood pressure for long term basis
what about NTS CVLM RVLM….??? this post was a total waste of time… sorry to say that !!!!
renin angiotensin aldosterone system
It wasn’t educative at all. It suddenly bycotted without a beginning and an end. Please consult essential of Medical Physiology for detailm
Baroreceptors are important for long term regulation of arterial pressure or not?
Stimulus to the body, activity , stress…etc activate a response in the low compliance baroreceptors of the arteries creating a action potential to either excite or inhibit heart rate and stroke volume for the needed adjustment.