What are the mechanisms that underlie the development of hypertension?
How is the sympathetic nervous system involved?
What does the Renin-angiotensin system have to do with anything? Watch and learn.
Intro
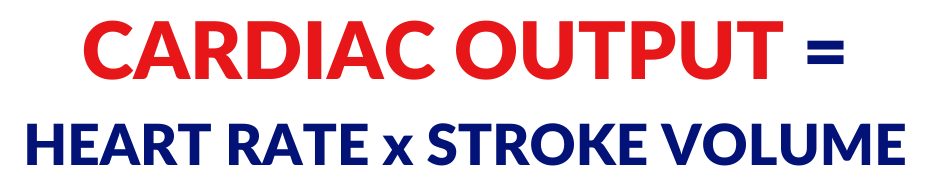
When it comes to the way hypertension develops, there are a number of different factors and in order to fully understand the factors, we have to do some Math. Math is always fun so, let’s talk about cardiac output.
Cardiac Output
Cardiac output refers to the amount of blood that each ventricle is pumping per minute. In order to calculate cardiac output, we need to take two factors into consideration.
Number one, the heart rate so, that’s the number of beats per minute and we’re going to multiply that by the stroke volume. That’s the amount of blood that each ventricle is pumping with each contraction.
Let’s take some simple numbers here. Let’s say, I have 70 beats per minute (70 bpm) and I multiply that by 70 mL. I am going to get, let’s say 4.9 L.
What’s the significance there?
Increased Blood Pressure
Well, when we come to blood pressure, blood pressure can be determined or calculated by taking cardiac output and multiplying that by peripheral resistance.
We already spoke about this cardiac output but, peripheral resistance deals with the amount of resistance to blood flow. If there is increased resistance to blood flow, it’s harder for the blood to get through the vessel, that is, an increase in peripheral resistance.
And, if you affect any of these two factors, you’re going to affect blood pressure.
Main Cause of Developing Hypertension: Increased Peripheral Resistance
When we’re dealing with hypertension, the main cause of increased blood pressure is going to be your peripheral resistance. There is something that is affecting the ability of the blood to flow through those vessels and that is going to increase your blood pressure.
The main reason for that is increased arteriolar vasoconstriction. We spoke about this a little bit in the previous video.
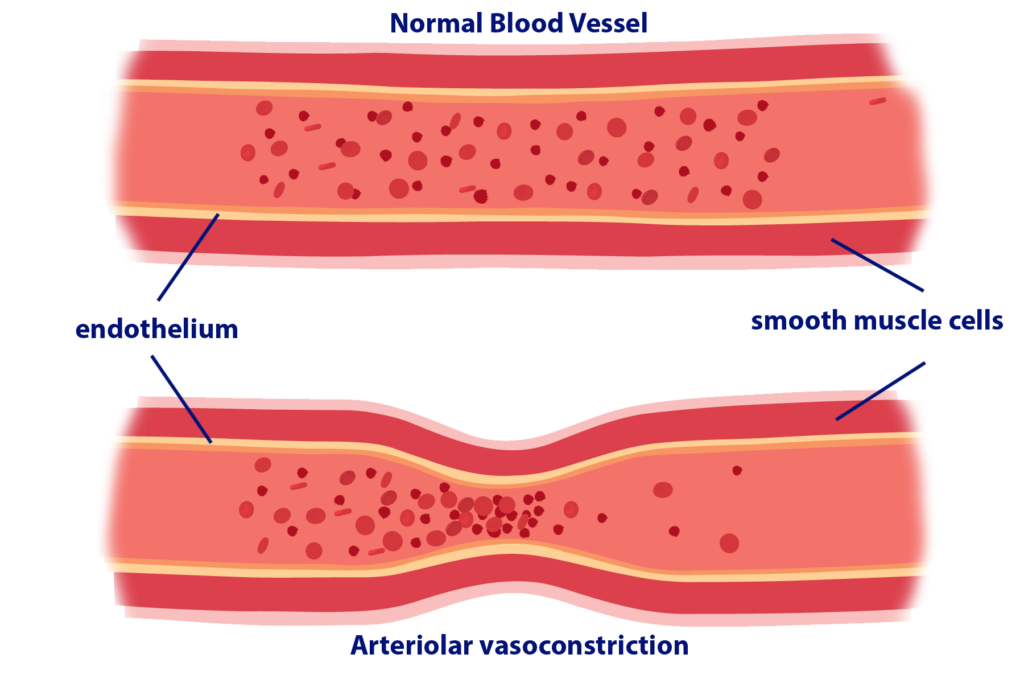
These are images of an artery– a normal artery and a vasoconstricted artery. The artery consists of an endothelial layer, and then, surrounding that is the smooth muscle layer.
Any time you hear muscle, you should think that there is a contraction that’s possible. So, if there is increased sympathetic activity, the sympathetic nervous system is releasing norepinephrine and epinephrine basically, adrenaline, that is going to cause contraction of that smooth muscle layer and as a result, what’s going to happen is the lumen of the arteries is going to get significantly smaller. As a result, you have less space for blood to flow through.
Think of it this way, if you have two tubes– one is wider, and the other is narrower, which one is going to be easier for water to flow through? Of course, the wider one because there’s more space. And, that’s the same way it is with the arteries.
If the arteries are narrower, you’re going to have more resistance to flow, increased peripheral resistance, and as a result, that’s going to cause an increase in blood pressure.
There are other factors that come into play.
If there’s increased peripheral resistance, that is going to make it harder for blood to flow to the destinations that it needs to go to. As a result of that, one of the places we’re going to see that effect is that there’s going to be decreased blood flow to the kidneys.
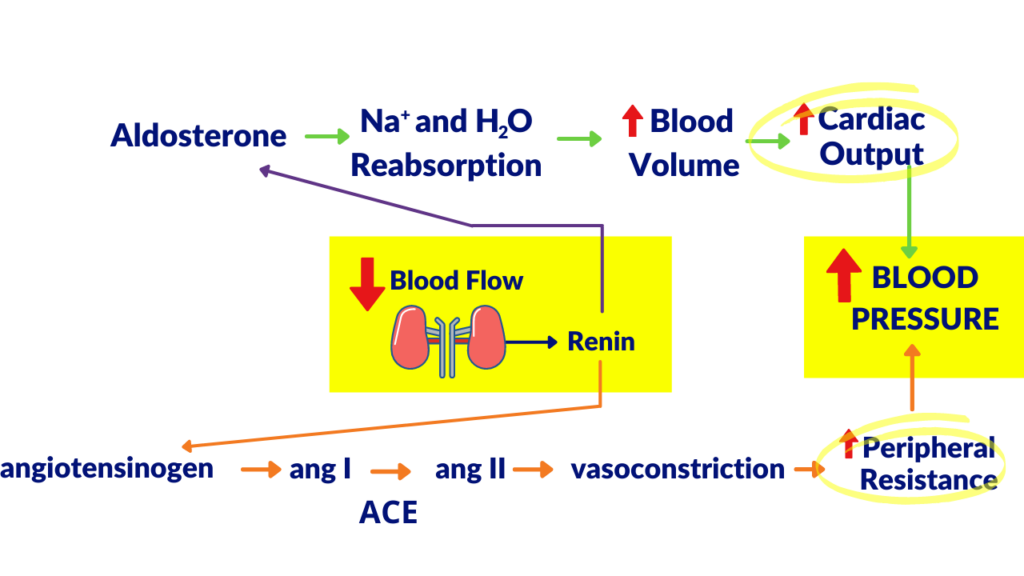
As a result of that decreased blood flow to the kidney, the kidney is going to release renin and that renin is going to have two main effects.
The Renin – Angiotensin System
What I’m describing here is going to be called the renin-angiotensin system. We’re going to have two different pathways that are going to be at play here.
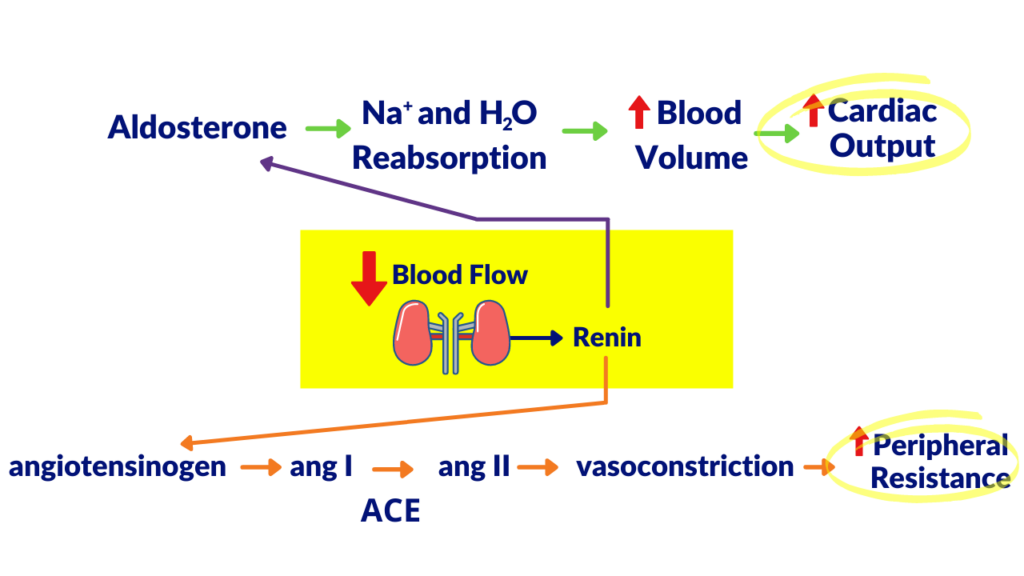
Pathway 1: Release of Angiotensinogen
Pathway number one is going to be that renin is going to cause angiotensinogen to be converted into angiotensin I. Angiotensinogen is an inactive protein that is produced in the liver. It gets converted to angiotensin I when the kidney releases renin.
Then, there’s an enzyme that is going to convert angiotensin I into angiotensin II. The name of that enzyme is ACE which stands for angiotensin-converting enzyme.
The significance here is that angiotensin II is going to be the most potent vasoconstrictor in the body. Of course, with increased vasoconstriction, what is that going to affect? That is going to affect peripheral resistance. That’s going to cause an increase in peripheral resistance.
Pathway 2: Release of Aldosterone
Renin also has another effect. It’s going to cause the release of aldosterone. The significance of aldosterone is that it is going to cause an increase in sodium ion reabsorption. A result of that is also H2O reabsorption.
What’s going to happen is it’s going to cause an increase in sodium ion reabsorption and the water is going to follow that sodium ion. This is all happening in the kidney and one of the main functions of the kidney is to filter the blood and to produce urine. So, we’re getting rid of waste. And, regulating the amount of water that leaves the body is very important in maintaining fluid balance in the body.
What happens if you’re reabsorbing more water into the body?
That is going to cause an increase in blood volume. As a result of that, if you have more blood and increased blood volume, when the heart contracts, it’s going to be sending more blood, and yes, you guessed it, that is going to cause an increase in cardiac output.
These both look very familiar to you right now and in red, I am going to show you that that is going to, these two factors are going to result in what? An increase in… blood pressure. How do we know that? Because we looked at that handy-dandy formula that was:
BP = CO x PR.
Because of that decrease in blood flow and that renin release, we’re activating these two different pathways that are going to result in increased cardiac output and increased peripheral resistance which in essence increases your blood pressure.
Now, here’s the problem.
If you’re increasing blood pressure even more, that can cause even more damage to the blood vessels. As a result of that, if we’re damaging the blood vessels, we also have a sympathetic activity that’s happening. That is going to cause a reduction in blood flow to the kidney.
You can see that this is a cycle and this is why hypertension is such a terrible thing because it kind of feeds on itself and makes itself worse.
In order to stop it, we need to stop this at one of these points depending on how bad it is. So, there are a number of places that we can stop this process and that’s exactly what we want to do.

amazing video! thanks !! :))
I don’t normally leave comments, but this is such an awesome explanation! I’ve been a nurse for 7 yrs and find myself back in school, your website and ability to break things down is genius!!! Thank you!!!!
Having Hypertension and never understanding the actual process, your breakdown explanation was extremely helpful and knowledgeable! Awesome! Thank you!
Outstanding! You have been blessed with explaining these matter in simplest form can’t stop watching and just putting down my text books and receiving more precise information this way. Thank you a whole bunch!
Great and detailed explanation!